Artificial intelligence is revolutionizing psychiatric care, transforming how mental health professionals diagnose, treat, and monitor patient conditions. Through advanced machine learning in healthcare, AI systems now analyze vast amounts of patient data – from speech patterns and facial expressions to electronic health records – detecting subtle signs of mental health conditions that human practitioners might miss.
The integration of AI in psychiatry represents a paradigm shift in mental healthcare delivery, offering 24/7 monitoring capabilities, personalized treatment recommendations, and early warning systems for crisis intervention. These technologies are particularly crucial in addressing the global mental health crisis, where traditional healthcare systems struggle to meet growing demand and many patients face barriers to accessing care.
From chatbots providing immediate emotional support to sophisticated algorithms predicting treatment outcomes, AI tools are becoming invaluable allies to mental health professionals. Yet, this technological revolution also raises important questions about patient privacy, the role of human connection in therapy, and the ethical implications of automated mental health care decisions.
As we stand at this intersection of technology and mental health, understanding how AI shapes psychiatric care becomes essential for healthcare providers, patients, and technologists alike.
How AI is Revolutionizing Psychiatric Diagnosis
Pattern Recognition in Patient Behavior
AI systems excel at identifying patterns in patient behavior that might be overlooked by human psychiatrists. Through advanced machine learning algorithms, these systems can analyze various data points, including speech patterns, facial expressions, and digital footprints from social media or smartphone usage.
For example, AI can detect subtle changes in a patient’s voice tone or speaking speed during therapy sessions, which might indicate shifts in emotional states. These systems process thousands of data points per session, creating detailed behavioral profiles that help track progress over time.
Natural Language Processing (NLP) enables AI to analyze text messages, social media posts, and journal entries for signs of mental health changes. The technology can identify linguistic patterns associated with depression, anxiety, or other conditions, often catching early warning signs before they become apparent through traditional observation methods.
Movement patterns and physical behaviors are also monitored through computer vision systems. These can detect changes in facial expressions, body language, and even micro-expressions that might signal emotional distress or improvement. When combined with other data sources, this creates a comprehensive view of patient behavior.
The real power lies in AI’s ability to correlate multiple behavioral indicators simultaneously, providing psychiatrists with data-driven insights that enhance their clinical judgment. This technology doesn’t replace human expertise but rather augments it with objective, quantifiable observations that support more accurate diagnoses and treatment plans.
Early Detection Systems
Artificial intelligence is revolutionizing how mental health professionals detect early warning signs of psychiatric conditions, potentially enabling intervention before symptoms become severe. Machine learning algorithms analyze various data points, including speech patterns, social media activity, and behavioral changes, to identify potential red flags that might go unnoticed in traditional psychiatric assessments.
For example, AI systems can detect subtle changes in a person’s typing speed, word choice, or social media posting frequency that may indicate the onset of depression or anxiety. These systems learn from vast datasets of patient information to recognize patterns associated with different mental health conditions, becoming increasingly accurate over time.
Smartphone applications equipped with AI capabilities now monitor users’ daily activities, sleep patterns, and communication habits. These apps can alert healthcare providers when they detect concerning changes in behavior, such as social withdrawal or disrupted sleep cycles, which often precede more serious mental health episodes.
Voice analysis technology has emerged as another powerful tool, with AI algorithms capable of identifying acoustic markers that may indicate emotional distress or the early stages of conditions like schizophrenia. By analyzing parameters such as pitch, rhythm, and verbal fluency, these systems can help identify individuals who might benefit from early intervention.
This technology is particularly valuable in reaching underserved populations and young people who might not otherwise seek traditional mental health services, making early detection more accessible and less stigmatizing.
AI-Powered Therapeutic Solutions
Virtual Therapy Assistants
Virtual therapy assistants, powered by advanced AI-powered conversational agents, are revolutionizing mental health support by providing accessible, 24/7 emotional assistance to those in need. These digital companions use natural language processing and machine learning algorithms to engage in meaningful conversations, offer coping strategies, and monitor users’ emotional well-being.
These AI assistants excel at providing initial mental health screening, guided meditation sessions, and cognitive behavioral therapy exercises. They can recognize patterns in users’ responses, track mood changes over time, and offer personalized suggestions for managing stress, anxiety, and depression. While they don’t replace licensed therapists, they serve as valuable supplementary tools, especially for individuals who face barriers to traditional therapy such as cost, location, or stigma.
Popular applications like Woebot and Wysa demonstrate the practical implementation of these virtual assistants. They employ evidence-based therapeutic techniques while maintaining a conversational, non-judgmental approach. The AI continuously learns from interactions, improving its ability to provide relevant support and recognize potential crisis situations that require professional intervention.
The effectiveness of these tools is particularly noteworthy in reaching younger generations who may feel more comfortable discussing their mental health through digital platforms. They also play a crucial role in preventive mental health care by helping users develop healthy coping mechanisms and emotional awareness before serious issues arise. As the technology continues to evolve, these virtual assistants are becoming increasingly sophisticated in their ability to provide personalized, culturally sensitive mental health support.

Personalized Treatment Plans
One of the most promising applications of AI in psychiatry is its ability to create highly personalized treatment plans for patients. By analyzing vast amounts of patient data, including medical history, genetic information, lifestyle factors, and treatment responses, AI algorithms can suggest tailored interventions that are more likely to succeed for each individual.
These AI-driven systems can identify patterns and correlations that might not be immediately apparent to human practitioners. For instance, they can predict which medications are most likely to be effective based on a patient’s specific symptoms and characteristics, potentially reducing the trial-and-error approach often used in psychiatric treatment.
Machine learning models can also adapt and refine treatment recommendations in real-time as new patient data becomes available. By continuously monitoring patient progress through digital tools and wearable devices, these systems can suggest adjustments to medication dosages, therapy approaches, or lifestyle modifications when needed.
The personalization extends beyond medication management. AI can recommend specific therapeutic techniques, optimal session frequencies, and even the most suitable therapist-patient matches based on communication styles and treatment preferences. For example, some patients might respond better to cognitive behavioral therapy, while others might benefit more from dialectical behavior therapy or mindfulness-based approaches.
Furthermore, AI-powered apps and digital platforms can provide personalized support between sessions, offering targeted coping strategies, mood tracking, and intervention suggestions based on individual trigger patterns and response histories. This continuous support helps bridge the gap between appointments and ensures that treatment remains responsive to the patient’s changing needs.
Real-World Implementation Challenges
Privacy and Data Security
The implementation of AI in psychiatry raises critical concerns about patient privacy and data security. As mental health data is among the most sensitive personal information, adhering to strict medical data protection standards is paramount. Healthcare providers must ensure that AI systems processing psychiatric data maintain HIPAA compliance and implement robust encryption protocols.
Key considerations include secure data storage, controlled access mechanisms, and transparent patient consent processes. AI systems often require large datasets for training, which necessitates careful anonymization of patient information while maintaining the data’s clinical relevance. Healthcare facilities must implement multi-factor authentication and regular security audits to prevent unauthorized access to AI-powered psychiatric platforms.
Another crucial aspect is the ethical handling of AI-generated insights. When AI systems identify patterns or make predictions about patient behavior, this information must be protected with the same rigor as traditional medical records. Healthcare providers should establish clear protocols for data sharing between AI systems and medical professionals while maintaining patient confidentiality.
Patients should also have control over their data, including the right to know how AI systems use their information and the ability to opt out of certain data collection practices. Regular updates to security protocols and staff training on data protection ensure that technological advancement doesn’t compromise patient privacy.
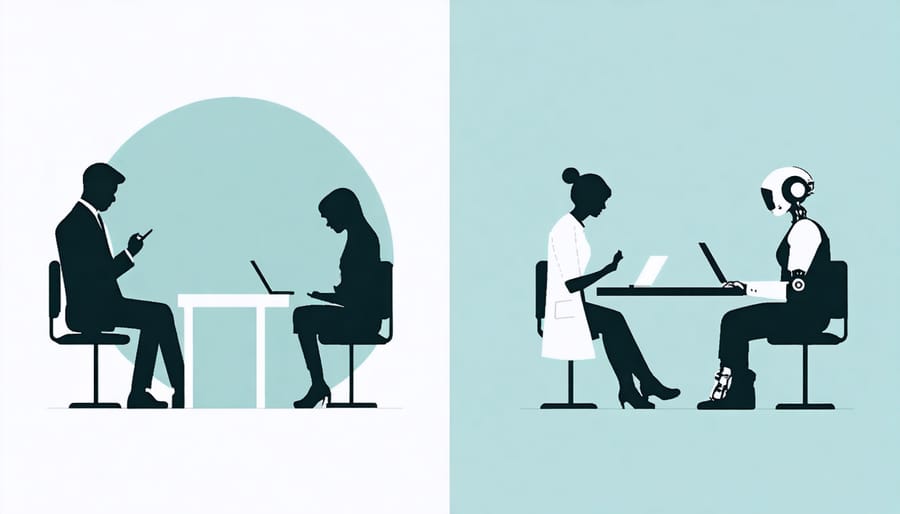
Integration with Traditional Care
The integration of AI tools in psychiatry doesn’t aim to replace human practitioners but rather to enhance their capabilities and improve patient care. AI systems serve as powerful assistants, helping psychiatrists manage routine tasks, analyze patient data, and identify patterns that might otherwise go unnoticed. This collaborative approach allows mental health professionals to focus more on what they do best: providing empathetic care and making complex clinical decisions.
For example, while AI can efficiently screen patients and suggest potential diagnoses, psychiatrists apply their expertise to validate these findings, consider individual patient circumstances, and develop personalized treatment plans. The human touch remains crucial in building therapeutic relationships, understanding nuanced emotional experiences, and providing contextual interpretation of AI-generated insights.
Many psychiatric practices have adopted a hybrid model where AI handles administrative tasks, monitors patient progress through digital platforms, and flags potential concerns, while psychiatrists maintain direct patient relationships and oversee treatment strategies. This integration has shown promising results in improving appointment efficiency, treatment adherence, and patient outcomes.
However, successful integration requires careful consideration of ethical guidelines, clear communication with patients about AI’s role in their care, and ongoing training for mental health professionals to effectively utilize these tools. The goal is to create a synergistic relationship where technology amplifies, rather than diminishes, the human elements of psychiatric care.
Future Prospects in AI Psychiatry
The future of AI in psychiatry holds immense promise, with emerging technologies poised to revolutionize mental healthcare delivery. As digital health innovations continue to advance, we’re likely to see more sophisticated AI-powered diagnostic tools that can detect subtle changes in patient behavior and emotional states through voice analysis, facial recognition, and natural language processing.
Machine learning algorithms are expected to become more precise in predicting mental health crises and potential relapses, enabling preventive interventions before situations escalate. These systems will likely integrate data from multiple sources, including wearable devices, social media activity, and electronic health records, to create comprehensive patient profiles and personalized treatment recommendations.
Virtual therapy assistants are anticipated to become more sophisticated, offering 24/7 support to patients while maintaining natural, empathetic conversations. These AI companions will work alongside human therapists, providing supplementary care and monitoring between sessions, rather than replacing human practitioners entirely.
We’re also likely to see advances in medication management, with AI systems helping psychiatrists optimize drug combinations and dosages based on individual patient characteristics, genetic markers, and treatment response patterns. This could significantly reduce the trial-and-error approach often associated with psychiatric medication.
Another exciting prospect is the development of AI-powered virtual reality environments for exposure therapy and skills training. These immersive experiences will be automatically adjusted based on patient responses and progress, creating truly personalized therapeutic experiences.
However, these advancements will need to address important considerations around privacy, ethical AI use, and maintaining the human element in mental healthcare. The focus will likely remain on creating tools that enhance rather than replace the therapeutic relationship, ensuring that technology serves to strengthen the connection between mental health professionals and their patients.
Artificial Intelligence continues to revolutionize psychiatric care, offering unprecedented opportunities for improved diagnosis, treatment, and patient support. The integration of AI technologies has demonstrated significant potential in early detection of mental health conditions, personalized treatment planning, and round-the-clock patient monitoring through digital platforms and apps.
As we look toward the future, AI-powered solutions are expected to become even more sophisticated, incorporating advanced natural language processing, emotion recognition, and predictive analytics to provide more accurate and timely interventions. These developments could help address the global shortage of mental health professionals while making psychiatric care more accessible and affordable for patients worldwide.
However, it’s crucial to maintain a balanced perspective. While AI shows immense promise, it should be viewed as a powerful tool to augment human psychiatrists rather than replace them. The human element – empathy, intuitive understanding, and complex decision-making – remains irreplaceable in mental health care.
Looking ahead, the successful implementation of AI in psychiatry will depend on continued collaboration between technology developers, mental health professionals, and regulatory bodies. This partnership will be essential in addressing ethical concerns, ensuring patient privacy, and maintaining high standards of care while leveraging AI’s capabilities to their fullest potential.
As this field evolves, we can expect to see more innovative applications that combine the best of human expertise with AI’s analytical power, ultimately working toward the common goal of better mental health outcomes for all.

